If a terminally ill patient meets the requirements to receive the medical aid-in-dying drugs, the patient and their attending physician must follow several steps which are carefully defined in the law, including:
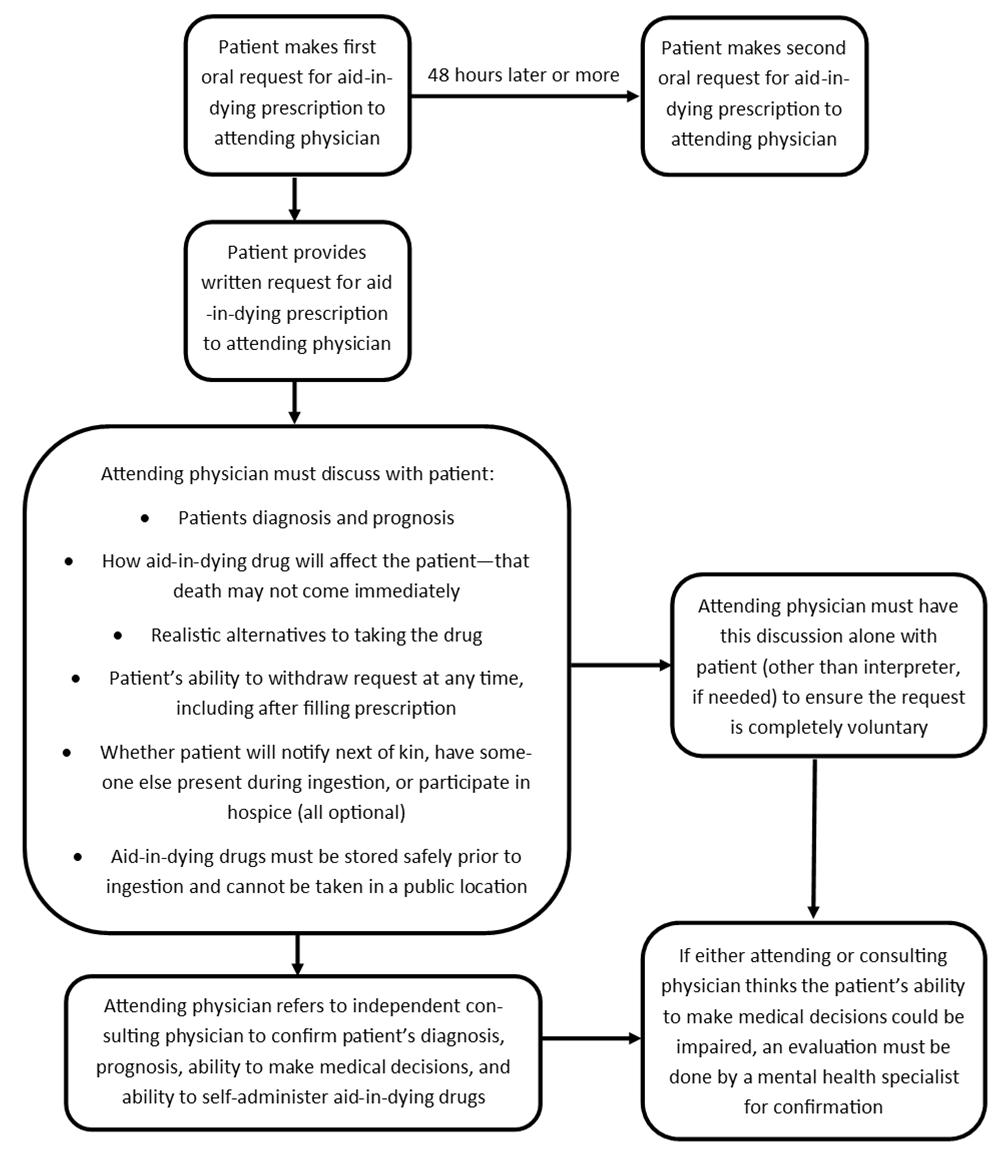
- The patient must make two oral requests, at least 48 hours apart, directly to their attending physician (the physician with primary responsibility for the care of the patient and treatment of their terminal disease).
- The patient must also make one request in writing, using the Patient’s Request for Aid-in-Dying Drug form (PDF). This form must be signed by the patient and two witnesses and provided directly to the patient’s attending physician. The law does not say specifically when the written request must be made.
- The physician must provide counseling to the patient regarding the items detailed below.
- The physician must discuss the aid-in-dying request with the patient without anyone else present (except an interpreter, if needed), to make sure the request is voluntary.
- The physician must refer the patient to a second, independent physician (a consulting physician). This physician must confirm the patient’s diagnosis, prognosis, ability to make medical decisions, and ability to self-administer the drugs.
If either physician thinks the patient’s ability to make medical decisions could be impaired, the patient must also see a mental health specialist (psychiatrist or licensed psychologist). The mental health specialist is only required to confirm the patient’s ability to make decisions.
Required Points of Discussion
The law requires that the attending physician and patient discuss a number of important topics, including:
- The patient’s diagnosis and prognosis
- How the aid-in-dying drug will affect the patient, and the fact that death might not come immediately
- Realistic alternatives to taking the drug, including comfort care, hospice care, palliative care, and pain control
- That the patient may, at any time, withdraw the request and that the patient may receive the drugs but decide not to take them
- Whether the patient will notify next of kin of their intention to take aid-in-dying drugs, have someone else present when taking the drugs, or participate in a hospice program. (The patient is not required to do any of these things.)
- That the patient should safely store the drugs prior to taking them and not take them in a public location
Once all these steps have been completed, the attending physician may provide the aid-in-dying drug by either dispensing it directly to the patient or by delivering the prescription to a participating pharmacist. By law, the physician cannot hand a written prescription directly to the patient or their representative.